


IMCB provides screening of a biologically active substance/extract/phytopreparation (on model reactions, mammalian cells and animal models) and consulting services for pharmaceutical and food industry, research institutes and individual research groups.
Based on the needs of the customer, services supplied by IMCB may range from single measurements to complete studies. Assays may be set up according to the requirements of the client. If necessary, we also assist in preparation of the material for publication of results.
The competence of IMCB is achieved and maintained by their active research. At present, research and development activities at IMCB are focused on oxidative stress and antioxidant functions.
We can assist our clients e.g. to investigate effects of plant extracts, phytochemicals, functional food and dietary supplements, on oxidation of LDL (® atherosclerosis) or DNA (® cancer), on cellular defence functions, and to explore antioxidant effects of intact plant/extract/ component/dietary supplement.
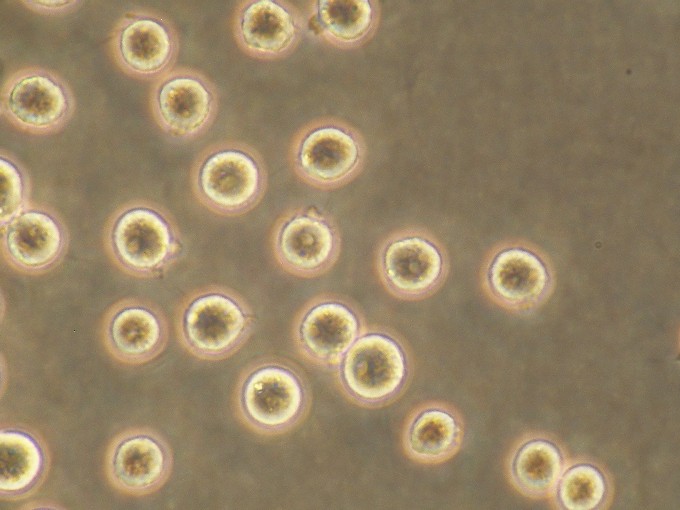
| Available cell systems: | ||||
| Human Hepatocytes |
 |
|||
| Rat Hepatocytes |
 |
|||
| Rat Neonatal Cardiomyocytes |
 |
|||
| Human Umbilical Vein Endothelial Cells - HUVEC | ||||
| Human Keratinocytes | ||||
| Human Fibroblasts | ||||
| Human Osteoblasts | ||||
| Cancerous cell lines - HepG2, SaOS, HL-60, T-REX HeLa, ... | |||
 |
 |
 |
 |
(i) Assessment of antioxidant potency
Focus
(i) Scavenging of free radicals
(ii) Prevention of lipid peroxidation
Models
(i) Screening of potency of the test compound in vitro
(ii) In vivo screening ®
demonstration of the effect on an animal model (rat, mouse) ®
placebo controlled studies with human volunteers
(iii) The use of oxidized LDL as bioindicators
Why antioxidant testing?
Purposeful and directed production of reactive oxygen species (ROS) is a key element of important physiological functions (signal transduction, apoptosis). Excessive production of ROS (e.g. due to chronic inflammation, ischemia, drugs, pollutants, irradiation, cigarette smoke etc.) may cause oxidative damage to cell constituents. Such changes may lead to mutagenesis, membrane disruption, receptor malfunction, altered enzyme activities and mitochondrial damage. ROS are known to be implicated in ageing processes, and in diseases the incidence of which typically increases with age (cancer, cardiovascular disease, neurodegenerative disorders). The potential beneficial effects of antioxidant compounds have led to intensive search for novel antioxidant molecules to be used as components of dietary supplement/functional food.
Assessment of antioxidant effect in vitro
Tests:
(i) Scavenging of 1,1-diphenyl-2-picrylhydrazyl radical (DPPH)
(ii) Scavenging of superoxide anion
(iii) Scavenging of peroxyl radical
(iv) Metal-chelating properties
(v) Electrochemical behaviour
(vi) Prevention of lipid peroxidation
Aim: To find out if the test compound/extract/phytopreparation can inactivate free radicals and/or prevent lipid peroxidation.
Procedure: DPPH radical, superoxide anion and peroxyl radical are produced by standard methods. Detection of free radicals is based on sensitive chemiluminescense techniques. Studies will be done with several concentrations of the test compound and repeated on separate days. The results will be presented as comparison of the potency of the test compound with that of a simultaneously tested known antioxidant. As the model of lipid peroxidation, peroxidation is induced chemically in biological lipids (e.g. lipids from rat liver).
Assesment of antioxidant effect in vivo
Tests:
(i) Total antioxidant capacity of plasma and liver tissues
(ii) Level of reduced glutathione in erythrocyte and liver cells
(iii) Level of lipid peroxidation products
(iv) Activities of antioxidant enzyme in erythrocytes and liver (SOD, glutathione peroxidase)
Aim: To find out if the test substance/extract/phytopreparation has antioxidant effects in vivo.
Procedure: Effect of the test compound/extract/phytopreparation will be investigated after induction of experimental oxidative stress (by vitamin E deficiency and/or chemical prooxidant) to mice/rats. The test compound will be administered with feed or drinking water. Markers of oxidative stress in various tissues will be determined at the end of the test period. Determination of test compounds in tissues, cells and extracellular fluid. Determination of total antioxidant capacity of plasma and tissues.
Implications
(i) Atherosclerosis, cardiovascular disease, injury process
Focus
(i) Oxidized LDL
(ii) Plasma lipids and lipoproteins
Models
(i) Screening
® animal modelWhy LDL oxidation?
For several years it has been known that development of atherosclerosis is related to the level of the ”noxious” low-density lipoprotein (LDL). More recent studies have revealed that ultimate atherogenic agents are in fact modified, mainly oxidized, forms of LDL. Clinical studies have shown that LDL-peroxidation products (LDL-PP) are closely related to coronary, carotid and brachial atherosclerosis. Indeed, as an indicator of the risk of atherosclerosis and cardiovascular disease (CVD) LDL-PP clearly exceeds sensitivity and specificity of the common lipid markers MDA/TBARS. Therefore, focusing on LDL oxidation will not only help in diagnosis and follow up of treatment of CVD, but also enables targeted development dietary supplements for prevention or decreasing the risk of atherosclerosis and CVD.
Prevention of LDL oxidation in vitro
Tests:
(i) Direct prevention of LDL oxidation (conjugated dienes, LDL lag phase)
(ii) LDL-incorporation.
Aim: To find out (i) if the test compound can prevent oxidation of human LDL in vitro, and (ii) if the test compound can incorporate into LDL particles.
Procedure: Studies are performed with LDL fraction isolated from human plasma. Oxidation is induced by copper and quantified by the common diene conjugation method. Studies will be done with several concentrations of the test compound and repeated on separate days. The results will be presented as comparison of the potency of the test compound with that of a simultaneously tested known antioxidant. Incorporation of test compounds into LDL to study the effect on LDL stabilisation.
Animal model: in vivo LDL oxidation and development of atherosclerotic lesions
Tests:
(i) Level of oxidized LDL
(ii) Stability of LDL against chemically induced oxidation
(iii) Effect of test compounds on atherosclerotic lesions
Aim: To find out how the test substance/extract/phytopreparation affects LDL oxidation and the progression of atherosclerosis in experimental animals
Procedure: Knockout LDLR mice (lacking the LDL receptor), fed an atherogenic diet, are used as an experimental model for atherosclerosis. The test compound will be administered in feed or drinking water. The level of LDL oxidation (circulating oxidized LDL) will be analyzed in blood samples. Atherosclerotic lesions will be recorded in histopathological investigations.
Effects on LDL oxidation in human volunteers
Tests:
(i) Level of total cholesterol
(ii) Level of LDL cholesterol
(iii) Level of oxidized LDL
Aim: To find out how the test compound affects LDL oxidation (and other lipid risk factors) in human body.
Procedure: Human volunteers with modestly elevated serum cholesterol level will be given the test compound or placebo after twelve-weeks run-in period. Blood samples will be taken at one to two week intervals during the study, and analyzed for LDL oxidation and the conventional plasma lipids.
Implications
(i) Chronic inflammations (rheumatoid arthritis, inflammatory skin diseases, psoriasis, Crohn’s disease, asthma, HIV), ischemia - reperfusion (infarction, stroke, organ transplantation)
Focus
(i) Production of reactive oxygen species by neutrophils and other cells of host defence
Models
(i) Screening ® demonstration of the effect in vivo (human volunteers)
Why cellular defence functions?
Generation of reactive oxygen species, hypochlorous acid and tyrosyl radical form together the basis of microbicidal action of human neutrophils. ROS production has been observed not only in neutrophils but also in macrophages, microglial cells of the brain, the Kupffer cells of the liver, monocytes, basophils, mast cells, and eosinophils. Besides the microbicidal action, reactive species generated by the oxidative burst and myeloperoxidase may cause damage to molecules and cellular components of the host organism. Prolonged overactivity of reactive species generating cell types results in sustained oxidative stress in a variety of inflammatory conditions: ischemia-reperfusion injury in myocardial infarction, stroke or transplantation, adult respiratory distress syndrome, rheumatoid arthritis, inflammatory bowel disease, HIV, psoriasis, and inflammatory conditions of the skin. Reactive species produced by the oxidative burst and myeloperoxidase activity are the ultimate damaging agents. It therefore seems logical that an effective inhibition of oxidative burst and myeloperoxidase activity would be a direct way for attenuation of the damage due to overactivity.
Effects on cellular defence functions in vitro
Tests:
(i)
Superoxide anion production (”oxidative burst”)
(ii) Hypochlorite production (myeloperoxidase
activity)
Aim: To find out how the test compound affects the ability of neutrophils (and other cells of the host defence) to produce reactive oxygen species in vitro.
Procedure: Studies are performed with human blood or cells isolated from human blood. Production of reactive oxygen species by stimulated neutrophils is recorded by chemiluminescence. Hypochlorite production (myeloperoxidase activity) is determined spectrophotometrically. Studies will be done with several concentrations of the test compound and repeated on separate days. The results will be presented as comparison of the potency of the test compound with that of a simultaneously tested known inhibitor of oxidative burst or myeloperoxidase activity.
Implications
(i) Genotoxicity, carcinogenesis
Focus
(i) Oxidative modification of DNA
Models
(i) Direct (in vitro) effect ® cell culture models ® animal models ® human volunteers
Why DNA damage?
Test:
(i) Determination of DNA damage by electrophoresis
Aim: To find out if the test compound causes oxidation of DNA or, alternatively, if the test compound can prevent experimentally induced DNA oxidation.
Procedure: The relative amount of 8-HdG is used as an index of DNA oxidation. Oxidation of chemically pure DNA and DNA in tissue homogenates will be monitored with time. Oxidation of DNA is induced experimentally by chemicals or irradiation. The results will be presented as comparison of the potency of the test compound with that of a simultaneously tested known antioxidant.
Tests:
(i)
Single-stranded DNA breaks by Comet assay
(ii)
DNA damage by electrophoresis
(iii) Determination of 8-HdG
Aim: To find out if the test compound causes DNA oxidation or, alternatively, if the test compound can prevent experimentally induced DNA oxidation in living cells.
Procedure: Studies will be done using a cell line suitable for the purposes of testing. DNA oxidation is induced experimentally by chemicals. The results will be presented as comparison of the potency of the test compound with that of a simultaneously tested known antioxidant.
Test:
(i) 8-HdG in leucocytes and tissues
Aim: To find out if the test compound causes DNA oxidation or, alternatively, if the test compound can prevent experimentally induced DNA oxidation in tissues of experimental animals.
Procedure: Studies will be done in animal models (usually rats or mice) that suit best for the purposes of testing. The test compound will be administered with feed or drinking water. DNA oxidation is affected experimentally by vitamin E deficiency and/or chemical prooxidant. At termination, DNA will be isolated from animal tissues and analyzed for the relative amount of oxidized DNA.
Implications
(i)
Drug-drug interactions
(ii)
Carcinogenesis
(iii) Cytotoxicity
Focus
(i)
Inhibition of specific activities of cytochromes P450 (CYP1A, 2A6, 2C9, 2D6,
2E1, 3A4)
(ii) Induction/repression of CYP 1A
Models
(i)
CYP activities in human liver microsomes
(ii) Hepatoma cell line HepG2 (alternative:
primary rat hepatocytes)
Why effects on CYP enzymes?
Phase I biotransformation is frequently the decisive step in obtaining beneficial vs adverse effects of a substance. Cytochromes P450 (CYP) is a superfamily of enzymes responsible for catalysis of reactions, usually hydroxylation, turning a hydrophobic compound into a more water soluble substance which can be excreted. CYP enzymes are present predominantly in liver but some, particularly CYP 1A, are found in extrahepatic tissues as well. Inhibition of CYP enzymes may cause adverse effects by changing pharmacological profile of a simultaneously applied drug. Same result is observed if expression of a particular CYP enzyme is changed by the compound/extract under investigation. CYP enzymes, and CYP 1A in particular, were implicated in carcinogenesis because of metabolising procarcinogens, e.g. polycyclic aromatic hydrocarbons, into carcinogenic substances. Similarly, harmless compounds may be metabolised into cytotoxic agents causing cell damage and necrosis/apoptosis.
Assessment of interaction with CYP enzymes
Test:
(i) Effect of the test substance/extract/phytopreparation on activities liver CYP family from microsomes
Aim: To find out whether substances/extracts inhibit specific activities of CYP enzymes in human liver microsomes.
Procedure: The following activities will be used: CYP 1A, 7-ethoxyresorufin de-ethylation; CYP 2A6, coumarin hydroxylation; CYP 2C9, diclofenac 4´-hydroxylation; CYP 2D6, AMMC hydroxylation; CYP2E1, nitrophenol hydroxylation; CYP 3A4, testosterone 6b-hydroxylation. Inhibition will be compared to known inhibitors of corresponding activities.
Induction/repression of CYP 1A in living cells
Tests:
(i)
Effect on expression of CYP in HepG2
(ii) Effect on expression of CYP in
primary rat hepatocytes
Aim: To test whether substances/extracts affect expression of CYP 1A.
Procedure: Human hepatoma cell line HepG2 expressing inducible CYP1A1 will be treated with known inducers for comparison. Expression of CYP 1A will be evaluated by Western blotting and specific activity measured directly in whole cells. Rat primary hepatocytes expressing inducible CYP 1A2 will serve as an alternative model.
Implications
(i) Biosafety
(ii) In
vitro toxicity
Focus
(i) Cytotoxicity (prooxidant activity)
(ii) Cytoprotectivity (elimination of
oxidative stress)
Models
(i) Primary cell culture (rat, pig and/or
human hepatocyte; rat cardiomyocyte)
(ii) Cell line (fibroblast (3T3 and Balb);
keratinocyte (HaCaT); endothelial cell (HUVEC); HL-60; HepG2; HeLa)
Why testing of cytotoxicity/cytoprotectivity?
In vitro screening of cytotoxic properties of the test substance/extract/phytopreparation can partially substitute in vivo test. Using primary cell cultures or cell lines derived from various sources opens a large variability of detection of cytotoxic properties of tested samples. On these cell models where pathological alterations (e.g. oxidative stress) had been induced, the cytoprotectivity of a compound/extract can be tested.
Assessment of cell toxicity/protectivity
Tests:
(i) Viability
- damage of cell membrane – leakage of LDH in medium; mitochondrial activity
measured by MTT assay (reduction of tetrazolium salt); Neutral red dye retention
assay; damage of mitochondria – leakage of AST
(ii) Redox
status of cell – content of glutathione
(iii) Energy
status of cell – intracellular level of ADP and ATP
(iv) Oxidative
damage of cell membranes – lipoperoxidation – assessed as TBARS
(v) Effect
on cell proliferation (DNA synthesis) – incorporation of bromo-deoxyuridine
into DNA by immunoassay
(vi) DNA
damage- single – stranded DNA breaks – Comet assay
Aim: To assess if the test substance/extract/phytopreparation will display cytotoxic/ cytoprotective effect against the oxidative stress induced in cells.
Procedure: Cell cultures will be used for the assessment of cytotoxicity and/or cytoprotectivity of substance/extract/phytopreparation. Their cytoprotective effect will be monitored on cell cultures intoxicated by model toxins, e.g. tert-butyl hydroperoxide or UV exposure. The cell viability, intracellular GSH, ADP and ATP level, and lipid peroxidation products will be used for the evaluation. Antiproliferative effect will be evaluated on proliferative cells by incorporation of bromo-deoxyuridine into DNA. DNA damage will be detected by Comet assay.
Implications
(i) Biosafety
(ii) In
vivo toxicity
(iii) Metabolization
Focus
(i) Safety
(ii) Oxidative
stress and related parameters
(iii) Detection and quantification of substances and
metabolites in body fluids, tissues and faeces
Models
(i) Experimental animals (rats, mice, pigs)
Why testing safety in vivo?
In vitro screening of cytotoxic properties of the test substance/extract/phytopreparation can only partially substitute in vivo tests. On the level of whole organism, many factors influence biological activity of substance/extract/phytoparation, e.g. bioavailability, excretion and metabolism.
Assessment of safety (biological activity)
Tests:
(i)
Health status monitoring. growth curves, feed consumption
(ii)
Macroscopic evaluation and histopathological
examination of organs
(iii) Parameters of clinical
biochemistry and hematology
(iv) Oxidative
stres related
parameteres
(v) DNA
damage- single – stranded DNA breaks – Comet assay
in peripheral lymphocytes, 32P-postlabeling of liver microsomal DNA
adducts
(vi) Content of
cytochrome P450 in liver microsomes
(vii)
Detection and quantification of substances and
metabolites in body fluids, tissues and faeces
Aim: To assess if the test substance/extract/phytopreparation will display effects on experimental animals.
Procedure: Experimental animals will receive the test substance/extract/phytopreparation as a feed additive. At the end of the feeding experiment, blood samples will be taken under anesthesia, organs of interest will be macroscopically evaluated and used for further examinations using the methods mentioned above.
Implications
(i) Biosafety
Focus
(i) Safety
(ii) Oxidative
stress and related parameters
(iii) Detection and quantification of substances and
metabolites in body fluids
Models
(i) Human volunteers
Why testing safety on human volunteers?
Safety testing on human volunteers serves for confirmation of results obtained on experimental animals and/or cell cultures. This confirmation is necessary because of existing inter-species differences in enzymatic systems, e.g. biotrasforming cytochromes P450.
Assessment of safety (biological activity)
Tests:
(i)
Health status monitoring, questionnaires
(ii) Parameters of clinical
biochemistry and hematology
(iii)
Oxidative
stres related parameteres
(iv) DNA
damage- single – stranded DNA breaks – Comet assay in peripheral
lymphocytes
(v) Detection and quantification
of substances and metabolites in body fluids
Aim: To assess whether the test substance/extract/phytopreparation will not display adverse effects on human volunteers.
Procedure: Human volunteers will be given the substance/extract/phytopreparation in the form of a food supplement. Questionnaires, medical examination, blood, and urine collection for determination of parameters of clinical biochemistry and hematology will be performed at the beginning, during and at the end of the study.
Contact:
Prof. RNDr. Jitka Ulrichová,
CSc.
Institute of Medical
Chemistry and Biochemistry (IMCB)
Hnývotínská 3, 775 15
Olomouc
Czech Republic
Tel/Fax
+420 585 632 312
E-mail
jitkaulrichova@seznam.cz